Signs of Damaged Skin Barrier & Dermatologist Repair Tips
11th Sep 2025
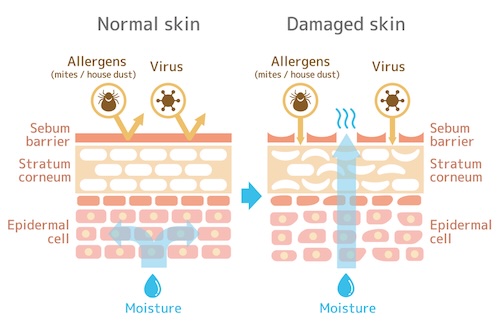 Your skin barrier is the micron-thin lipid wall on the very surface of your skin; when it’s intact, water stays put and microbes stay out. When that wall cracks, a chain reaction of dryness, redness, bumps, and unexpected breakouts starts almost overnight. This article pinpoints the 15 clearest warning signs that your barrier has reached that tipping point—and, more importantly, shares repair strategies dermatologists trust and use themselves.
Your skin barrier is the micron-thin lipid wall on the very surface of your skin; when it’s intact, water stays put and microbes stay out. When that wall cracks, a chain reaction of dryness, redness, bumps, and unexpected breakouts starts almost overnight. This article pinpoints the 15 clearest warning signs that your barrier has reached that tipping point—and, more importantly, shares repair strategies dermatologists trust and use themselves.
Why focus on the barrier first? Because every serum, moisturizer, or spot treatment you buy can only work if this outer shield is healthy. A strong barrier prevents moisture loss, blocks pollution and allergens, and calms the immune responses that cause itch and inflammation. Below, you’ll find an easy-to-scan list of symptoms, followed by a science-backed recovery plan you can start tonight. Ready to check your own skin’s security system? Let’s get into the signs.
1. Chronic Dryness and Tightness
Persistent dryness that refuses to budge is often the first heads-up your skin gives that its protective wall is faltering.
What It Looks & Feels Like
Skin feels like it's shrinking a size after every wash. It can look paper-dry, slightly dull, and may even crease when you smile. Moisturizer offers brief relief but tightness creeps back within an hour.
Why Barrier Damage Causes It
When ceramides and cholesterol in the stratum corneum run low, water evaporates faster—a process measured as transepidermal water loss (TEWL). Healthy skin sits around 5–15 g/m²/hr; compromised barriers rocket above 25 g/m²/hr, leaving cells shriveled and rigid.
Simple At-Home Check
Lightly pinch the skin on your cheek or inner forearm for two seconds, then release. If the fold is slow to spring back and feels papery, dehydration and a struggling barrier are likely culprits.
2. Flakiness and Visible Scaling
Notice specks of “face dandruff” on your collar or a foundation that clings to patchy spots? That’s your stratum corneum shedding unevenly instead of in invisible sheets—a classic sign of a weakened skin barrier.
Surface Clues
- Fine, white or off-white flakes on cheeks, brows, and around the nose
- Larger plate-like scales on arms or shins that lift when scratched
- Makeup or sunscreen gathers in tiny islands, highlighting roughness
Underlying Mechanism
Ceramides act like mortar between skin cells. When they’re depleted, corneocytes detach too soon, creating visible debris. Elevated TEWL plus low natural moisturizing factors (NMF) turn those loose cells into dry scale.
What to Rule Out
If flakes are greasy and yellow, think seborrheic dermatitis; silvery plaques with clearly defined edges may signal psoriasis. Persistent thick scaling, bleeding, or joint pain warrants a quick dermatologist visit for proper diagnosis.
3. Sudden or Persistent Redness
Among the most obvious signs of damaged skin barrier is redness that shows up uninvited and overstays its welcome. If your cheeks look flushed hours after exercise or you wake up blotchy despite a gentle routine, your capillaries are sounding the alarm.
Visual Traits
- Diffuse pink or crimson tone that covers entire cheeks or forehead
- Patchy blotches shaped like islands, sometimes warm to the touch
- “Hot face” sensation after cleansing, showering, or stepping into wind
Inflammation Pathway
When the lipid wall cracks, allergens and pollutants slip inside, kicking off a cytokine cascade. Those chemical messengers tell blood vessels to widen, so more immune cells rush in—leaving skin visibly red and feeling warm.
Trigger Tracking Tip
Snap a quick phone photo whenever redness spikes and jot down what you used or ate in the last six hours. A two-week diary often reveals repeat offenders—think spicy food, new cleanser, or a windy commute.
4. Burning or Stinging With Normal Products
If your go-to lotion or even plain tap water suddenly feels like acid, your skin barrier is waving a red flag: its buffer is gone and nerves are exposed.
Immediate Symptoms
- Sharp, prickling heat within seconds of cleanser, toner, or sunscreen
- Redness that lingers up to an hour after rinsing
- “Water burn” sensation in the shower or pool
Sensory Nerve Hypersensitivity
A thinned lipid layer no longer insulates C-fiber nerve endings. Small pH changes, alcohol, or fragrance now trigger exaggerated pain signals, making everyday formulas feel harsh.
Patch-Test Protocol
Apply a rice-grain of product to a 2 cm spot behind the ear. Wait 24 hours; if no sting or redness appears, try the same patch on your jaw before full-face use.
5. Itchiness (Pruritus)
Hallmark Signs
- Persistent urge to scratch, especially after showers or at night
- Fine red lines or sheet marks where you’ve rubbed the skin
- Tiny scabs from “mindless” scratching that never seem to heal
Biochemical Causes
A compromised barrier leaks water and allows irritants in, prompting mast cells to dump histamine. At the same time, lower levels of natural moisturizing factors (NMF) leave nerve endings exposed, making even a light fabric brush feel like fiberglass.
Soothing Techniques
Press a cool compress for 5 minutes, then follow with a thick, fragrance-free emollient rich in colloidal oatmeal or panthenol. Keep nails short, run a humidifier above 40 % RH, and switch to cotton or bamboo sheets to cut friction while you sleep.
6. Rough or Bumpy Texture
Run your fingertips across your cheek or the back of an arm—if it feels like fine-grit sandpaper instead of silk, your barrier has likely lost some of its structural glue. These tiny bumps can crop up even when the skin looks “normal” from a distance, making makeup sit unevenly and body lotion pill.
How It Manifests
- Pin-head-sized plugs that look like gooseflesh or keratosis pilaris
- Foundation gathers around pores, highlighting an orange-peel effect
- Skin snags on washcloths and catches light unevenly
Lipid Matrix Breakdown
When the 3:1:1 ratio of ceramides, cholesterol, and fatty acids is off, corneocyte edges curl upward. The lifted edges trap keratin and dead cells, creating a grid of micro-bumps you can feel but barely see.
Gentle Resurfacing Advice
Once itching or redness has calmed, introduce a low-strength lactic acid or gluconolactone (≤ 5 %) twice a week. Follow immediately with a ceramide-rich cream to replenish lipids, and avoid physical scrubs that can shear off the fragile barrier you’re trying to rebuild.
7. Unexplained Acne Flares or Pustules
A breakout that appears out of the blue—especially in zones you almost never see pimples—often signals a barrier that no longer keeps acne-causing microbes in check.
Clinical Presentation
Clusters of tiny whiteheads, papules, or tender pustules pop up on cheeks, temples, and even neck folds. They feel sore, drain quickly, and reform within days.
Barrier–Bacteria Connection
When the acid mantle creeps above pH 5.5, lipophilic Cutibacterium acnes multiplies and biofilms flourish. Simultaneously, gaps in the lipid matrix let inflammatory molecules seep deeper, turbo-charging each lesion.
Product Audit
Park anything with heavy mineral oil, drying alcohol, or > 5 % benzoyl peroxide for now; swap in non-comedogenic glycerin serums and ceramide creams until balance returns.
8. Post-Inflammatory Hyperpigmentation That Lingers
When a pimple or bug bite leaves a shadow that won’t fade, your barrier is lagging in the repair race. Derms call this post-inflammatory hyperpigmentation (PIH), and it often drags on in darker skin tones.
Visible Clues
- Flat brown, gray, or purplish spots cling to the former blemish
- Color barely lightens after four weeks
- Darkens again with brief sun exposure
Impaired Regeneration
Leaky lipids slow the enzymes that shed old cells, so melanin stays trapped longer and spots linger. Fresh collagen also stalls, giving discoloration no scaffold to renew on.
Brightening Safely
Stick to 2 % niacinamide and licorice root, wear SPF 50 daily, and delay strong acids until skin stops stinging.
9. Dull, Lackluster Complexion
Skin that looks flat and gray—even under bright natural light—usually means the outer barrier is scattering light instead of reflecting it. No highlighter can fake radiance when that microscopic film is compromised.
How to Identify
Compare cheeks to inner arm at noon; a sallow face and lost “glow line” signal a lackluster complexion.
Oxygen & Lipid Deficit
Slow microcirculation deprives cells of oxygen while ceramide gaps lift corneocyte tiles, diffusing light like frosted glass and amplifying dullness.
Quick Revive Tactics
- Spritz glycerin-panthenol mist, then lock it with ceramide cream.
- Slug a petrolatum “button” on high points overnight for bounce.
- 60-second facial massage boosts blood flow; add omega-3 fish weekly.
10. “Squeaky-Clean” Tight Feeling After Cleansing
That too-fresh, almost rubbery squeak you hear when fingertips glide across your face isn’t a victory lap for hygiene—it’s a warning that your cleanser just stripped vital barrier lipids.
Immediate Sensation
- Skin feels two sizes too small within minutes of toweling off
- Cheeks squeak audibly when you run a finger across them
- Fine lines look deeper until moisturizer is applied
Surfactant Stripping
High-pH soaps and sulfates dissolve the intercellular “mortar,” raising TEWL and spiking the classic signs of damaged skin barrier—dryness, redness, and sting—before you even reach for toner.
Swap Suggestions
- Choose pH-balanced (4.5–5.5) gel, cream, or oil cleansers
- Limit cleansing to 60 seconds; mornings can be water-only rinses
- Look for gentler surfactants like cocoyl isethionate and added glycerin
11. Fine Lines That Seem to Appear Overnight
Waking up to creases that weren’t there last night is jarring, but these sudden lines are usually a dehydrated barrier crying for help.
Visual Indicators
- Hair-fine lines appear like dry riverbeds after flying
- Press-and-hold test erases folds within seconds
- Concealer pools in creases by noon
Dehydration Lines vs. True Wrinkles
Permanent wrinkles stay when skin is stretched; dehydration lines disappear because they sit only in the thirsty topmost cell layer.
Fast Fix
Mist humectant serum on damp skin, follow with ceramide cream, and seal trouble spots overnight with a pea-size dab of petrolatum.
12. Discoloration and Blotchy Patches
Blotchy reds, browns, and ashy spots that change hourly often signal a struggling barrier—one of the sneakiest signs of damaged skin barrier.
Spotting the Sign
Uneven tone shows up as pink islands next to pallid zones or shadowy brown smudges that darken after sun. Makeup sits unevenly, amplifying the patchwork effect.
Vasodilation + Melanocyte Stress
A leaky barrier lets irritants spark cytokine-driven vasodilation—hello redness—while oxidative stress overstimulates melanocytes, pumping out melanin in bursts. The double hit yields both red and brown discoloration.
Calming Ingredients
Layer creams with bisabolol, 0.5 % centella asiatica extract, and green-tea polyphenols. These quell inflammation, down-regulate tyrosinase, and gradually even tone without bleaching or irritation.
13. Increased Skin Sensitivity to Sun, Wind, or Temperature Swings
If a mild breeze feels like sandpaper or winter air pricks like needles, your barrier has lost its built-in thermostat. Without that lipid coat, nerves sit closer to the surface and over-react to even slight shifts in climate.
Everyday Clues
- Face stings in cold air within seconds
- Instant flushing under a heat lamp or morning sun
- Red, tight skin after moving from an air-conditioned office to humid outdoors
Thermoregulation Role of Barrier
A healthy barrier slows water loss and insulates micro-vessels, helping skin keep a steady ~33 °C. Once compromised, it can’t buffer temperature spikes, so nerves and vessels fire stress signals that show up as redness and pain.
Protective Measures
- Apply broad-spectrum mineral SPF 30+ year-round
- Wrap scarves or wear brimmed hats to cut wind shear
- Run an indoor humidifier > 40 % RH and limit hot showers to 5 minutes
- Reapply ceramide cream every four hours during extreme weather
14. High Trans-Epidermal Water Loss (TEWL) You Can Feel
Sometimes moisturizer evaporates before you screw the cap back on; that rapid “drink-then-desert” effect is soaring trans-epidermal water loss (TEWL), proof your skin’s brick-and-mortar wall has gaps and needs repair. It literally leaks valuable water.
Practical Observations
- Skin feels parched within an hour of moisturizing, demanding repeated top-ups
- Lips chap, cuticles crack, and clothes lint clings to shins by mid-day
Measuring TEWL
Curious numbers? Pocket TEWL pens run under \$50 and display g/m²/hr; derm clinics use corneometer scans to compare you with healthy baselines.
Humectant-Occlusive “Sandwich”
Morning and night, layer a glycerin or panthenol serum, follow with ceramide-rich cream, then press a pea-size petrolatum “button” onto cheeks and around eyes to lock moisture in.
15. Recurring Minor Infections or Rashes
When your barrier is down, opportunistic microbes seize the moment. That’s why the same small rash or folliculitis patch keeps circling back no matter how many creams you try.
What Happens
- Razor bumps turn into pustular folliculitis week after week
- Cold sores, impetigo crusts, or ringworm spots pop up in familiar places
- Heat rash or diaper-like chafing appears after a single sweaty workout
Barrier as Immune Shield
Healthy skin hosts Langerhans cells that spot invaders early and lipids that maintain an antimicrobial pH (~5). Breaches raise surface pH and thin that immune sentry line, letting bacteria, fungi, and viruses multiply unchecked.
When to Seek Professional Help
See a dermatologist right away if you notice red streaks, spreading pus, fever, or lesions that enlarge after 48 hours. Quick prescription care plus barrier repair prevents chronic scarring and systemic infection.
16. Dermatologist-Approved Repair Guide: 6 Essential Steps
Checked off more than a handful of the signs of damaged skin barrier above? A “product diet” paired with strategic replenishment will speed recovery and prevent the cycle from repeating. The six steps below follow the order most board-certified dermatologists use in clinic—remove triggers first, then rebuild, then carefully layer back in performance actives.
Step 1 – Stop the Offenders
Your barrier can’t rebound while the very things that broke it are still in play.
- Park high-strength retinoids (
> 0.3 %), peel pads, and toners with alcohol denat. - Skip essential oils, menthol, eucalyptus, and scrubs with nut shells or sugar granules.
- Limit cleansing to twice a day max; no midday “refresh” wipes.
- Dial exfoliating devices (Clarisonic, spinning brushes, foreo) down to zero.
Give skin a two-week vacation from these known irritants before moving to Step 2.
Step 2 – Use a pH-Balanced, Barrier-Supporting Cleanser
Cleansing is non-negotiable but must be barrier-friendly.
- Aim for formulas with a final pH between
4.5and5.5. - Star ingredients: glycerin, beta-glucan, panthenol, oat extract.
- Night routine: a gentle oil or micellar first if you wear SPF/makeup, followed by a creamy surfactant cleanser for ≤ 60 seconds.
- Morning routine: lukewarm water rinse or a single swipe of the same mild cleanser.
Pat dry—no rubbing—and move to moisturization within 60 seconds (“damp-skin rule”).
Step 3 – Rebuild Lipids With the Right Moisturizer
Think of this as laying fresh bricks and mortar.
- Scan the INCI list for the ideal
3 : 1 : 1ratio (ceramides : cholesterol : fatty acids). - Added niacinamide (
≤ 2 %) supports ceramide synthesis without sting. - Texture matters: lotion for oily/combo skin, cream for normal/dry, balm for eczema-prone areas.
- Apply a nickel-size amount face + neck, quarter-size per limb, twice daily.
Stick with one formula for at least 28 days—the average epidermal turnover—before judging results.
Step 4 – Seal With Occlusives at Night
Moisturizer supplies the lipids; an occlusive keeps them and the water in place.
- Classic petrolatum (if acne-safe for you) cuts TEWL by up to 99 %.
- Alternatives: squalane balm, dimethicone silicone gel, shea-butter sticks.
- “Slugging” lite method: after moisturizer, dot a pea-size amount on cheeks, around eyes, and over any flaky patches—no need to coat the whole face.
- Wash pillowcases twice a week to avoid trapped bacteria.
Step 5 – Re-Introduce Actives Slowly
Once sting, tightness, and redness have been tamed for seven straight days, you can add back performance ingredients.
- Start with barrier-friendly options:
1–2 %niacinamide serum or a0.1–0.3 %retinal. - Follow the 3-day rule—add one new active, use it every third night, and monitor for 72 hours before adding or increasing frequency.
- Graduate to PHAs, then mild AHAs/BHAs if no flare-ups occur.
- Keep pH-sensitive actives (vitamin C, exfoliating acids) in a different time slot from retinoids to lower irritation risk.
Step 6 – Lifestyle Choices That Accelerate Repair
Topicals do the heavy lifting, but daily habits decide how fast you heal.
- Eat omega-3-rich foods (salmon, chia seeds) 3× per week to boost lipid synthesis internally.
- Drink ~2 L water daily; dehydration raises TEWL.
- Run a cool-mist humidifier to maintain indoor RH above 40 %, especially in winter or air-conditioned offices.
- Cap recreational screen time at 7 hours; blue-light stress ups reactive oxygen species.
- Manage cortisol with 7–8 hours of sleep, breathing exercises, or short walks.
Consistency here can shave weeks off the repair timeline.
FAQ Corner (Clinics Hear These Every Day)
Will my barrier heal itself if I just wait it out?
Mild damage can normalize in one skin-renewal cycle (~28 days), but moderate to severe disruption may take 8–12 weeks without targeted care. The six steps above accelerate that process.
Can azelaic acid hurt or help?
Formulations at ≤ 10 % are generally barrier-friendly and even calm redness. Prescription-strength (15–20 %) can sting compromised skin; wait until burning and flaking subside before use.
How do I know I can stop “slugging”?
When moisturizer keeps skin comfortable for 8 hours and makeup no longer pills, you can dial occlusives down to every other night.
Follow these guardrails and your outer shield will come back thicker, smoother, and far less reactive—setting the stage for any future glow-up goals.
17. Skin Barrier Health Starts Today
Dryness that won’t quit, redness that won’t fade, and products that suddenly sting are your skin’s “check-engine” lights; park the irritants, switch to a pH-balanced cleanser, rebuild with ceramides, seal with an occlusive, re-introduce actives slowly, and back it all up with sleep, omegas, water, and humidity. Follow that six-step rhythm for one full cell-turnover cycle and most barriers bounce back smoother, calmer, and far more resilient.
Need a deeper dive or just moral support while you heal? Browse the science explainers and real-life success stories on the Mollenol site, and drop your email for our no-spam newsletter—fresh dermatologist tips delivered only when they’re worth your time.
