What Causes Folliculitis? Triggers, Risks & Prevention Tips
16th Sep 2025
 Folliculitis is simply inflammation of a hair follicle, and it usually springs up when staph bacteria sneak through a tiny nick or clogged pore. Less often, fungi, viruses, friction, shaving, heavy oils, or tight clothing set the stage for those itchy red bumps.
Folliculitis is simply inflammation of a hair follicle, and it usually springs up when staph bacteria sneak through a tiny nick or clogged pore. Less often, fungi, viruses, friction, shaving, heavy oils, or tight clothing set the stage for those itchy red bumps.
The good news is that most cases stay superficial and clear quickly once you pinpoint the trigger and make a few small changes. Whether your bumps appear after a hot-tub soak, a close shave, or a sweaty workout, understanding the why is the first step toward keeping your skin calm. In the sections that follow, we'll separate infectious from non-infectious causes, map out the biggest risk factors, show you how to tell folliculitis from look-alike rashes, and lay out everyday habits that stop it from coming back. By the end, you’ll know exactly when a home remedy suffices and when a dermatologist’s visit is smarter.
Folliculitis Explained: Inflammation of a Hair Follicle
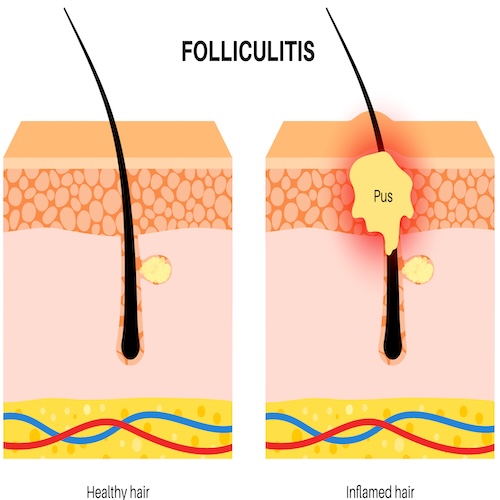
Folliculitis occurs when the tiny pocket that holds a hair becomes inflamed—red, swollen, sometimes pus-filled. Because hair covers almost the whole body, the rash can show up on scalp, beard, buttocks or anywhere between. Understanding what causes folliculitis starts with a quick tour of follicle anatomy. Dermatologists list the condition among their most common skin complaints. When bumps last only days it’s called acute; if they linger or recur for months, it’s chronic and the root trigger needs tracking down.
Hair Follicle Anatomy 101
A follicle is a narrow tube sunk in the dermis. At its base sits the bulb, the factory for new hair cells. Halfway up, a sebaceous gland drips sebum into the canal, then the tube narrows and exits the skin surface. That opening is barely wider than a pinhead, so friction, sweat, or a wandering germ easily wedges inside and irritates the lining.
From Irritation to Infection: The Inflammatory Chain Reaction
- A nick, heat rash, or clogged oil duct injures the follicle opening.
- Microbes or chemicals slip into the moist tunnel.
- Your immune system rushes white cells to the scene.
- Pus and fluid collect, lifting a small red or yellow bump.
- Nearby skin turns tender and itchy until the blockage clears.
Infectious Culprits: Bacteria, Fungi, Viruses & Parasites
When people ask “what causes folliculitis most of the time?” the answer is simple—an infection. Micro-organisms that normally coexist peacefully on your skin seize the opportunity once a follicle is nicked, clogged, or softened by moisture. The invader type determines how the rash looks, feels, and responds to treatment, so it helps to know the usual suspects.
Bacterial Folliculitis (Staphylococcus aureus & Pseudomonas)
Staph aureus tops the list. It hides on healthy skin and inside noses, waiting for a chance to slip through micro-tears from shaving, scratching, or tight clothing. The result: clusters of itchy, white-tipped bumps that pop up fast and sometimes crust.
“Hot-tub” folliculitis, by contrast, is triggered by Pseudomonas aeruginosa thriving in warm, under-chlorinated water. Lesions erupt 8–48 hours after a soak, often on areas trapped under swimwear.
Quick tips
- Use a new, sharp razor every 5–7 shaves.
- Shower and change out of swim gear promptly.
- If outbreaks keep recurring, ask your provider about a nasal mupirocin course to reduce staph carriage.
Fungal & Yeast-Related Folliculitis
When antibiotics, heavy sweating, or occlusive clothing upset the skin’s microbiome, yeasts such as Malassezia (a.k.a. pityrosporum) can overgrow—especially on the upper back, chest, and hairline. Candida species behave similarly in moist folds. These bumps are usually uniform, itchy, and may worsen with standard acne antibiotics.
Clues you’re dealing with fungus
- Rash improves after antifungal shampoo or cream.
- Papules feel sand-papery rather than pustular.
- You’ve been on recent oral antibiotics or systemic steroids.
Viral & Parasitic Causes (Less Common)
Herpes simplex can inflame follicles around the mouth or genitals, producing grouped blisters instead of classic pustules. Molluscum contagiosum—small, waxy bumps with a central dimple—is sometimes misidentified as folliculitis but is caused by a poxvirus, not bacteria.
Parasites are rare yet possible. Demodex mites living in facial follicles may ignite rosacea-like eruptions, while exposure to infested animals can introduce larva migrans, creating serpiginous tracks rather than discrete pustules.
Because infectious triggers differ, cultures or scrapings guide therapy. When bumps don’t resolve with basic care, a dermatologist’s swab can pinpoint the microbe and fast-track the right treatment.
Non-Infectious Triggers & Everyday Irritants
Sometimes the answer to “what causes folliculitis?” is plain old irritation rather than germs. Anything that scrapes, blocks or overheats the follicular opening can spark the same red, pimple-like bumps even when no bacteria are in charge. Pinpointing these lifestyle culprits is often the fastest way to stop repeat flare-ups.
Shaving, Waxing & Plucking
A razor gliding too close can nick the canal or make curly hairs curl back under the skin—a twin recipe for pseudofolliculitis barbae. Hot wax and aggressive tweezing yank the shaft, leaving a microscopic wound.
Quick fixes
- Shave in the direction of hair growth with a sharp, single-blade razor.
- Prep skin with a lubricating gel and rinse the blade after every pass.
- Consider electric clippers, depilatory cream or professional laser for stubborn beard bumps.
Friction & Occlusion from Clothing or Gear
Tight yoga pants, shoulder straps or helmet liners trap sweat and rub the same patch for hours. The repeated micro-trauma inflames follicles while the moist environment keeps them swollen.
Tips
- Opt for moisture-wicking, loose-fit fabrics during workouts.
- Remove sweaty gear ASAP and shower within 30 minutes.
- Wash athletic wear in fragrance-free detergent to avoid chemical residue.
Oils, Heavy Cosmetics & Comedogenic Skin Care
Thick balms, petrolatum, butters and heavy silicones can form an airtight seal. Heat and bacteria build underneath, leading to clogged follicles that look like acne but sting like folliculitis.
Ingredient watch-list
- Mineral oil, lanolin, cocoa butter, dimethicone in high amounts.
- Swap for “non-comedogenic,” oil-free or gel-based formulas.
Medications & Topical Steroids
Long-term oral steroids, immunosuppressants, and over-the-counter steroid creams thin the skin’s defenses, making follicles more reactive to minor insults. If bumps appear after starting a new drug, flag it for your prescriber.
Underlying Medical Conditions
Diabetes, obesity, chronic acne, or HIV can tilt the immune balance so that even small irritations blossom into a rash. Good glucose control, weight management and routine skin checks reduce episodes.
Who Gets It? Key Risk Factors & Vulnerable Groups
Anyone with a hair follicle can develop folliculitis, but patterns emerge when doctors look at clinic data. Hormones, lifestyle, and even the weather tilt the odds, turning an everyday pore into a red, itchy bump. Knowing where you land on the risk spectrum lets you tweak habits before trouble starts.
Age, Sex & Hair Type
- Teens and twenty-somethings pump out extra sebum, creating a sticky playground for bacteria.
- Men with coarse, curly beard hair often battle razor-induced bumps, while women may notice flare-ups on legs after shaving.
- Post-menopausal estrogen decline thins skin and slows healing, so minor friction can spark chronic folliculitis.
Occupation & Athletic Activities
Jobs requiring tight uniforms, helmets, or occlusive PPE—think healthcare, food service, firefighting—rub and trap sweat all shift long. Athletes who live in spandex or share mats, pools, or hot tubs (swimmers, wrestlers, triathletes) add extra heat and microbes to the mix.
Climate & Seasonal Elements
Hot, humid weather floods follicles with sweat and friction; outbreaks surge every summer in the Southeast and Gulf Coast. Winter isn’t foolproof either—cold, dry air cracks skin, giving staph an easy entrance under bulky layers that chafe.
Spotting the Bumps: Recognizing Folliculitis vs. Look-Alikes
Before you can fix the problem, you have to know what you’re looking at. Folliculitis typically centers on a single hair, but several other rashes—acne, heat rash, even some infections—mimic its angry red dots. Use the checkpoints below to decide whether the bumps on your skin match classic folliculitis or warrant a different game plan.
Classic Signs & Symptoms
- Pin-head–size red papules or white-tipped pustules with a hair in the center
- Itching, stinging, or mild tenderness that worsens with friction
- Clusters appear suddenly after shaving, sweating, or hot-tub exposure
- Usually stays superficial; squeezing may release a tiny tuft of hair and pus
Conditions Commonly Confused with Folliculitis
| Look-alike | Key Clue it’s Not Folliculitis |
|---|---|
| Acne vulgaris | Lesions include blackheads/whiteheads; no central hair |
| Keratosis pilaris | Rough, sand-paper bumps on outer arms/thighs; rarely itch |
| Molluscum contagiosum | Dome-shaped, flesh-colored bumps with central dimple |
| Shingles | Painful, nerve-band rash that blisters rather than pustules |
| Heat rash (miliaria) | Tiny, clear vesicles after heavy sweating; no pus |
When It Might Be an STD
Genital bumps are most often simple folliculitis from shaving or tight underwear. Still, herpes simplex (grouped blisters that ulcerate) or early syphilis (single painless ulcer) can masquerade as inflamed follicles. If lesions recur, spread beyond hair-bearing areas, or coincide with fever or swollen glands, schedule STI testing instead of self-treating.
Daily Habits to Prevent Future Flare-Ups
The surest way to break the cycle is to remove as many day-to-day triggers as possible. Small tweaks in hygiene, grooming, and lifestyle cut the odds that bacteria or friction will get another shot at your follicles. Think of the tips below as a checklist—stacking even a few of them often keeps bumps away for good.
Hygiene & Shower Etiquette
- Shower within 30 minutes of sweating, swimming, or hot-tubbing.
- Use a gentle antibacterial or 4% benzoyl-peroxide wash on prone areas.
- Pat—don’t rub—skin dry and assign each family member their own towel.
Smart Shaving & Hair Removal Routine
- Always start with warm water and a slick shave gel to soften hairs.
- Glide a sharp, single- or double-blade razor with the grain in one pass.
- Rinse the blade in alcohol afterward; swap it out every 5-7 shaves.
- Explore electric clippers, depilatory creams, or laser if razor bumps persist.
Clothing & Laundry Choices
- Opt for loose, moisture-wicking fabrics during workouts and sleep.
- Peel off sweaty gear ASAP; wash it in fragrance-free detergent and hot water.
- Rotate backpacks, purse straps, and helmet liners to prevent constant rubbing on the same spot.
Skin-Care & Product Selection
- Check for “non-comedogenic” on lotions, sunscreens, and makeup.
- Skip thick petrolatum, lanolin, and heavy silicones on folliculitis-prone zones.
- Leave-on products with salicylic acid, niacinamide, or tea tree oil keep pores clear without stripping skin.
Diet, Stress & Immune Support
- Hydrate and aim for a plate rich in zinc, omega-3 fats, and colorful produce.
- Manage stress with sleep, exercise, or meditation—cortisol spikes impair skin defense.
- If you have diabetes or another immune-altering condition, strict medical control further lowers flare odds.
Consistently following these habits tackles what causes folliculitis at its root—paving the way for smoother, calmer skin year-round.
Treatment & When to Call the Dermatologist
Most short-lived outbreaks clear with simple TLC, but lingering or severe cases need a targeted plan. Use the quick guide below to decide whether you can treat bumps at home or should tap a skin-care pro.
At-Home First Aid for Mild Cases
- Wash the area twice daily with a gentle antiseptic or benzoyl-peroxide cleanser.
- Apply a warm, moist compress for 10 minutes to loosen trapped hairs and soothe pain.
- Dab on an over-the-counter antibiotic ointment or diluted tea-tree oil 2× daily.
- Cover tender pustules with a thin hydrocolloid patch to absorb drainage and curb picking.
- Pause shaving or friction-heavy activities until skin is smooth again.
Red Flags Warranting Medical Attention
Seek prompt evaluation when you notice:
- Rapid spread, deep painful nodules, or fever/chills.
- Red streaks or swelling that hint at cellulitis.
- Bumps that return monthly, scar, or resist one week of OTC care.
- Immunocompromised status, uncontrolled diabetes, or recent chemotherapy.
Early intervention prevents boils, scarring, and needless discomfort—so don’t hesitate to book that dermatology visit if any warning sign pops up.
Moving Forward with Clearer Skin
Folliculitis rarely shows up out of nowhere. Once you know whether bacteria, yeast, shaving habits, or sweaty gear is the culprit, you can tackle the root and keep flare-ups from cycling back. Start by protecting the follicle—swap in looser fabrics, smarter shave techniques, and non-clogging skin care. Cleanse promptly after workouts, use targeted over-the-counter treatments early, and don’t ignore warning signs that warrant a dermatologist’s eye. With those small, consistent tweaks, most people see bumps calm down quickly and stay that way. Curious about gentle, plant-based options that fit into this routine? Visit the Mollenol homepage to explore solutions designed for sensitive, bump-prone skin.
