The Three-Layer Architecture of Human Skin
19th Aug 2025
 Human skin represents one of the body's most sophisticated organ systems, comprising three distinct layers that work synergistically to protect, regulate, and maintain overall health. Each layer—the epidermis, dermis, and hypodermis (subcutaneous tissue)—possesses unique structural characteristics and specialized functions that contribute to the skin's remarkable versatility as both a barrier and a dynamic biological interface[1][2].
Human skin represents one of the body's most sophisticated organ systems, comprising three distinct layers that work synergistically to protect, regulate, and maintain overall health. Each layer—the epidermis, dermis, and hypodermis (subcutaneous tissue)—possesses unique structural characteristics and specialized functions that contribute to the skin's remarkable versatility as both a barrier and a dynamic biological interface[1][2].
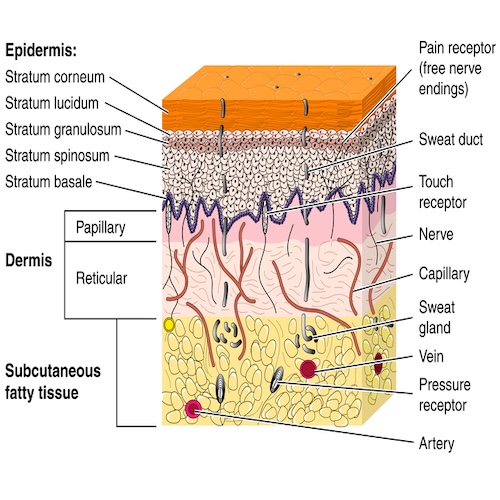
Cross-sectional illustration of the skin showing the epidermis, dermis, and hypodermis layers with hair follicles, sweat glands, nerves, and blood vessels.
The Epidermis: The Protective Outer Shield
The epidermis forms the outermost layer of skin, serving as the body's primary defense against environmental threats[1][2]. This remarkable structure, measuring between 0.03 to 2 millimeters thick depending on body location, functions as a waterproof barrier while contributing to skin tone and appearance[3][4].
Structural Organization
The epidermis consists of five distinct sublayers arranged from deepest to most superficial[1][5]:
- Stratum basale: The deepest layer containing stem cells that continuously proliferate
- Stratum spinosum: The thickest epidermal layer with newly formed keratinocytes
- Stratum granulosum: Contains keratinocytes with specialized granules for barrier formation
- Stratum lucidum: Present only in thick skin areas like palms and soles
- Stratum corneum: The outermost protective layer of dead, flattened cells[4]
Cross-sectional microscopic illustration of human skin layers highlighting epidermal strata and key cells such as keratinocytes, melanocytes, and Merkel cells.
Cellular Components and Functions
The epidermis houses several specialized cell types that contribute to its protective functions[1]:
Keratinocytes constitute the predominant cell population, producing keratin proteins and essential lipids that form the epidermal water barrier[1]. These cells undergo a continuous 30-day migration process from the basal layer to the surface, where they are shed as part of the skin's renewal cycle[5].
Melanocytes synthesize melanin pigment, providing natural protection against ultraviolet radiation. These cells transfer melanin granules to surrounding keratinocytes through specialized cellular processes[1].
Langerhans cells serve immunological functions, acting as antigen-presenting cells that help detect and respond to potential threats[5].
The Critical Barrier Function
The epidermis performs multiple essential barrier functions that are crucial for survival[6][7]:
- Physical Protection: The stratum corneum employs a "brick and mortar" model, where protein-rich corneocytes (bricks) are surrounded by specialized lipid matrices (mortar)[6][7]
- Water Regulation: The lipid matrix, dominated by ceramides, cholesterol, and free fatty acids, prevents excessive water loss while maintaining proper hydration[7][8]
- Chemical Barrier: Maintains an acidic pH (around 5.5) that supports beneficial microbial communities while deterring harmful pathogens[9]
- Immune Defense: Contains antimicrobial peptides and supports the skin's microbiome ecosystem[6]
The Dermis: The Structural Foundation
Located beneath the epidermis, the dermis provides the structural backbone of skin, measuring 20 to 30 times thicker than the epidermis at 0.5 to 4 millimeters thick[2][10]. This layer houses the skin's vascular networks, nerve systems, and appendages while providing mechanical support[11][12].
Architectural Divisions
The dermis comprises two functionally distinct regions[13][14]:
Papillary Dermis forms the upper, thinner layer composed of loose connective tissue. This region contains fine collagen type III fibers, elastic fibers, and forms the dermal papillae that interdigitate with epidermal ridges[13][15]. The papillary dermis is highly vascularized with capillary loops that supply nutrients to the avascular epidermis and facilitate thermoregulation[13].
Reticular Dermis constitutes the deeper, thicker layer containing dense irregular connective tissue. This region features coarse collagen type I fiber bundles arranged in a meshwork pattern, providing the skin's primary tensile strength and elasticity[13][14]. The reticular dermis houses larger blood vessels, lymphatic networks, and extends into the subcutaneous layer[13].
Specialized Fibroblast Populations
Recent research has revealed that papillary and reticular dermis harbor phenotypically distinct fibroblast populations with specialized functions[16][17]:
Papillary fibroblasts demonstrate greater proliferative capacity and secrete angiogenic factors including VEGF, IGF-1, and Angiopoietin-1. These cells show enhanced ability to support capillary network formation and epidermal-dermal communication[16][17][18].
Reticular fibroblasts produce higher levels of structural proteins including collagen I and laminin, while secreting different growth factors such as HGF and FGF-2. These cells provide the primary mechanical support structure for the skin[16][17].
Skin Appendages and Support Systems
The dermis houses essential skin appendages that contribute to skin function[19][20]:
Hair Follicles extend from the epidermis deep into the dermis and sometimes into the hypodermis. These structures contain hair root plexuses that serve as sensitive mechanoreceptors[21][20].
Sweat Glands include two types: eccrine glands for thermoregulation distributed across most body surfaces, and apocrine glands associated with hair follicles in specific regions that respond to emotional stimuli[19][22].
Sebaceous Glands produce sebum, an oily secretion that lubricates hair and skin while providing antimicrobial properties[19][20].
Sensory Networks
The dermis contains sophisticated sensory receptor systems that enable tactile perception[23][21]:
Mechanoreceptors include Meissner's corpuscles for light touch, Ruffini endings for skin stretch and pressure, and Pacinian corpuscles for vibration detection[23][21].
Thermoreceptors detect temperature changes, with cold receptors most active around 77°F and heat receptors responding to temperatures above normal body temperature[23].
Detailed anatomical illustration of human skin showing epidermis, dermis, and hypodermis layers with labeled structures including dermal papilla.
The Hypodermis: The Insulating Foundation
The hypodermis, also known as subcutaneous tissue, forms the deepest skin layer and serves as the interface between skin and underlying structures[11][2]. This layer varies significantly in thickness across body regions and between individuals[12].
Composition and Structure
The hypodermis primarily consists of adipose tissue organized into lobules separated by connective tissue septa[11][24]. This layer contains:
- White adipocytes for energy storage and insulation
- Loose areolar connective tissue with collagen and elastic fibers
- Blood vessels and lymphatic networks
- Nerve fibers extending to upper skin layers
- Some skin appendages like deep hair follicles[11][12]
Functional Roles
The hypodermis performs several critical functions[24][25]:
- Energy Storage: Adipocytes store lipids as triglycerides, serving as the body's primary energy reserve[24]
- Thermal Insulation: The fatty layer helps maintain body temperature and protects against heat loss[11][25]
- Mechanical Protection: Provides cushioning against physical trauma and impact[11][24]
- Endocrine Function: Secretes hormones including leptin and adiponectin that regulate metabolism and satiety[24][25]
- Structural Mobility: The loose arrangement of fibers allows skin to move freely over underlying muscle and bone[11]
Integration and Clinical Significance
The three skin layers function as an integrated system where disruption in one layer can significantly impact overall skin health[26][27]. Understanding this architecture has profound implications for skincare product development, wound healing, and dermatological treatments[28][29].
Recent advances in 3D bioprinting technology have emphasized the importance of recreating all three layers in skin equivalents, as full-thickness models demonstrate superior functionality compared to partial constructs[26][27]. Research shows that the presence of the hypodermis layer significantly influences gene expression patterns related to skin hydration, development, and differentiation[26].
The skin's barrier function relies on the coordinated interaction between layers, with the epidermis providing the primary protective barrier, the dermis supplying structural support and vascular networks, and the hypodermis offering insulation and energy storage[7][30]. This sophisticated three-layer system enables human skin to serve as both a protective shield and a dynamic interface with the environment, making it one of the body's most remarkable and essential organs.
Detailed anatomical illustration of the skin showing the epidermis, dermis, and hypodermis layers with hair follicles, sweat glands, and various other structures labeled.
This comprehensive understanding of skin layer architecture continues to drive innovations in dermatological research, therapeutic approaches, and the development of advanced skin care formulations that can effectively interact with and support each layer's unique functions and requirements.
⁂
Mollenol's Multi-Layer Mechanism of Action in Skin
Mollenol represents a sophisticated natural antimicrobial formulation that targets multiple skin conditions through its strategic interaction with all three skin layers. The product's effectiveness stems from its synergistic blend of botanical active compounds that work at different levels of skin architecture to address bacterial infections, inflammation, and barrier dysfunction[96][97].
Core Active Ingredients and Their Properties
Mollenol's therapeutic efficacy is built upon four primary botanical antimicrobials[96][97]:
Clove Bud Oil (Rich in Eugenol and Acetyl Eugenol) - Comprising the primary active component, eugenol constitutes 71-90% of clove oil and demonstrates potent membrane-disrupting bactericidal properties[98][99]. Research shows eugenol achieves a minimum inhibitory concentration (MIC) of 0.31 mg/mL against Cutibacterium acnes, the primary acne-causing bacteria[96].
Coconut-Derived Lauric Acid - This medium-chain fatty acid exhibits selective lytic action against Gram-positive bacteria with an MIC of 1.95 µg/mL against C. acnes, making it approximately 15 times stronger than benzoyl peroxide[96][100]. Lauric acid's unique molecular structure allows efficient skin barrier penetration while supporting lipid layer integrity[100][101].
Tea Tree Oil (Terpinen-4-ol) - The active compound terpinen-4-ol provides bactericidal, anti-inflammatory, and antioxidant properties. Clinical trials demonstrate that 5% tea tree oil gel reduced total acne lesion counts and severity 3-6 times more effectively than placebo over 45 days[96][102][103].
Sandalwood Oil - Contributing additional anti-inflammatory and wound-healing sesquiterpenes, sandalwood oil provides supportive therapeutic effects through traditional medicinal pathways[96].
Interaction with the Epidermis
Stratum Corneum Penetration Enhancement
Mollenol's formulation leverages the penetration enhancement properties of its essential oil components to overcome the skin's primary barrier. Research demonstrates that clove oil achieves an enhancement ratio (ER) of 2.63 for drug penetration, significantly outperforming synthetic enhancers like azone (ER 1.97)[104][105].
The mechanism involves disruption of stratum corneum lipid structure rather than permanent damage. Eugenol enhances skin penetration of diverse compounds by temporarily altering the highly ordered intercellular lipid matrix, creating channels for active ingredient delivery[106][99][107].
Lauric acid's dual action proves particularly effective in the epidermis by:
- Strengthening the lipid barrier through incorporation into the stratum corneum's "brick and mortar" structure[100]
- Penetrating efficiently due to its medium-chain fatty acid structure that balances molecular size with bioactivity[101]
- Targeting acne-causing bacteria specifically, with research showing significant bactericidal activity against Cutibacterium acnes[100][108]
Antimicrobial Activity Against Epidermal Pathogens
The active compounds in Mollenol demonstrate multi-target antimicrobial mechanisms:
Eugenol damages bacterial membranes through hydrophobic penetration of lipopolysaccharide cell walls, causing structural alterations and intracellular component leakage[109][110]. Studies show eugenol can inhibit membrane-bound ATPase activity in pathogenic bacteria while generating reactive oxygen species (ROS) that disrupt cellular processes[109].
Terpinen-4-ol from tea tree oil exhibits broad-spectrum antimicrobial activity, with research confirming effectiveness against Staphylococcus aureus, S. epidermidis, and Propionibacterium acnes[102][103]. The compound demonstrates lower MIC values for P. acnes than staphylococci, making it particularly suitable for acne treatment[102].
Dermal Layer Interactions
Anti-Inflammatory Mechanisms
Mollenol's components target the inflammatory pathways within the dermis that contribute to acne pathogenesis. The formulation addresses the four interlocking pathogenic pillars of acne: hyper-seborrhoea, hyper-keratinisation, bacterial overgrowth, and inflammation[96].
Eugenol provides COX-2 inhibition for anti-inflammatory activity while offering mild local anaesthetic effects[96][99]. This dual action helps reduce both the inflammatory response and associated discomfort from active lesions.
Lauric acid supports dermal healing by calming inflammatory pathways and helping to restore barrier function damaged by acne treatments or over-cleansing[100]. Its anti-inflammatory properties make it particularly suitable for sensitive or reactive skin types.
Supporting Dermal Repair Processes
The botanical compounds in Mollenol contribute to wound healing and tissue regeneration within the dermal layer:
Tea tree oil components demonstrate antioxidant properties that help neutralize free radicals contributing to inflammatory damage[103]. Research shows tea tree oil can reduce inflammatory lesion counts, particularly papules and pustules[103].
Sandalwood oil sesquiterpenes provide additional wound-healing support through traditional medicinal pathways, though clinical evidence for the complete formulation requires further research[96].
Hypodermis and Systemic Considerations
Penetration Depth and Systemic Absorption
The volatile nature and small molecular size of essential oil components allow for deeper skin penetration beyond the epidermis[107][111]. However, Mollenol's formulation is designed for topical antimicrobial action rather than systemic absorption.
Essential oils are naturally volatile and do not accumulate in the body, being easily eliminated through feces and urine[112]. This characteristic makes them safer alternatives to synthetic antimicrobials that may cause systemic side effects with prolonged use.
Supporting Subcutaneous Health
While Mollenol primarily targets epidermal and dermal layers, its anti-inflammatory properties may provide indirect benefits to subcutaneous tissue by reducing overall inflammatory burden and supporting healthy circulation in deeper skin layers[96].
Clinical Application Strategy
Targeted Delivery System
Mollenol employs a multi-pronged approach to maximize therapeutic effectiveness:
Direct Application - The lotion is applied as a thin smear directly to lesions, with users reporting faster "head-softening," reduced redness, and accelerated pustule drying within several days[96][113].
Occlusive Enhancement - Mollenol Hydrocolloid Patches infused with tea tree and clove oils provide additional antimicrobial support while creating a moist healing environment that enhances active ingredient penetration[114][115][116].
Barrier Protection - The patches serve a dual function by containing pus to prevent spread while maintaining optimal healing conditions through hydrocolloid technology[115][116].
Synergistic Mechanisms
The combination of active ingredients provides coverage across all four pathogenic pillars of acne development[96]:
- Antimicrobial Action: All three primary components demonstrate proven efficacy against C. acnes
- Anti-inflammatory Effects: Eugenol, lauric acid, and terpinen-4-ol all contribute inflammation reduction
- Barrier Support: Lauric acid specifically strengthens skin barrier function
- Penetration Enhancement: Essential oil components facilitate deeper active delivery
Laboratory studies demonstrate synergistic effects between these components, suggesting the complete formulation may provide enhanced efficacy beyond individual ingredient contributions[96].
Mechanism Summary and Clinical Positioning
Mollenol's effectiveness across skin layers stems from its evidence-based selection of botanical antimicrobials that individually match or outperform standard topical agents in laboratory studies[96]. The formulation's strength lies in its multi-target approach that addresses bacterial proliferation, inflammation, and barrier dysfunction simultaneously.
Mollenol's natural composition and low resistance potential make it a valuable addition to acne management protocols, offering antimicrobial efficacy with reduced risk of bacterial resistance compared to conventional antibiotic treatments[96][117].
- https://www.semanticscholar.org/paper/44d65213997d3898f3aa7047385c003f7b79d097
- https://journals.sagepub.com/doi/10.1177/08853282241276799
- https://www.semanticscholar.org/paper/c040c85e8348da63db02b68c6fc432deb26c6f6b
- https://link.springer.com/10.1007/978-981-19-7415-1_15
- https://pubs.aip.org/apb/article/5/4/046103/149642/A-suspended-layer-additive-manufacturing-approach
- https://research.tue.nl/en/publications/skin-layer-mechanics(68fd0390-64d9-4dce-b84d-b7ca787594c4).html
- https://www.semanticscholar.org/paper/49b82e949b12311bbd99c874210b9eaf784e1870
- https://www.semanticscholar.org/paper/c2a50eddf488dbef8fe77b25497e7134a14f48d4
- https://www.nature.com/articles/s42003-024-07106-4
- https://onlinelibrary.wiley.com/doi/10.1002/adhm.201801019
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10373447/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11105295/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11756454/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4437818/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4793052/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10623945/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9860843/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3385954/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4038073/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8002265/
- https://www.ncbi.nlm.nih.gov/books/NBK470464/
- https://www.utmb.edu/pedi_ed/CoreV2/Dermatology/page_03.htm
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8583944/
- https://www.ncbi.nlm.nih.gov/books/NBK441980/
- https://www.verywellhealth.com/skin-anatomy-1068880
- https://pubmed.ncbi.nlm.nih.gov/22507037/
- https://journals.cambridgemedia.com.au/wpr/volume-32-number-1/anatomy-physiology-and-function-all-skin-layers-and-impact-ageing-skin
- https://journals.cambridgemedia.com.au/download_file/8270/3917
- https://www.smileworksliverpool.co.uk/blog/epidermal-barrier-function/
- https://www.dermcoll.edu.au/atoz/skin-structure-function/
- https://www.youtube.com/watch?v=xUW3E6eDbzU
- https://dermnetnz.org/topics/skin-barrier-function
- https://www.skindepth.com.au/blogs/news/layers-of-the-skin
- https://www.biotechmedjournal.com/articles/abb-aid1026.php
- https://xlink.rsc.org/?DOI=D2BM02022J
- https://karger.com/article/doi/10.1159/000029897
- https://www.mdpi.com/1422-0067/23/19/11651
- https://www.mdpi.com/1422-0067/23/20/12654
- https://linkinghub.elsevier.com/retrieve/pii/S0022202X18325569
- http://biorxiv.org/lookup/doi/10.1101/2020.11.29.402594
- https://app.jove.com/t/59372
- https://www.jvas.in/article/histological-studies-on-the-dermis-of-different-breeds-of-dogs
- https://www.science.org/doi/10.1126/science.432659
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9848196
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8764052/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6346526/
- https://www.mdpi.com/1422-0067/16/12/26078/pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3280198/
- https://www.mdpi.com/2073-4409/8/6/607
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10368082/
- https://www.mdpi.com/2218-273X/10/12/1607/pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6736903/
- https://www.elsevier.com/resources/anatomy/integument/dermis/papillary-and-reticular-layers-of-dermis/15106
- https://www.uniprix.com/en/tips/3/dermo-cosmetic/skin-appendages
- https://www.nature.com/articles/ijo2013200
- https://www.kenhub.com/en/library/anatomy/papillary-layer-of-dermis
- https://en.wikipedia.org/wiki/Skin_appendage
- https://www.kenhub.com/en/library/anatomy/adipose-tissue
- https://www.kenhub.com/en/library/anatomy/reticular-layer-of-dermis
- https://www.ncbi.nlm.nih.gov/books/NBK482278/
- https://en.wikipedia.org/wiki/Adipose_tissue
- https://www.ncbi.nlm.nih.gov/books/NBK535346/
- https://my.clevelandclinic.org/health/body/24052-adipose-tissue-body-fat
- https://en.wikipedia.org/wiki/Dermis
- https://karger.com/chapter/doi/10.1159/000441540
- https://anndermatol.org/DOIx.php?id=10.5021/ad.23.078
- https://www.tandfonline.com/doi/full/10.1080/21688370.2024.2361197
- https://onlinelibrary.wiley.com/doi/10.1111/exd.14895
- https://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2010.02326.x
- https://onlinelibrary.wiley.com/doi/10.1111/exd.12296
- https://www.jstage.jst.go.jp/article/oleoscience/17/11/17_539/_article/-char/ja/
- https://www.mdpi.com/2079-9284/11/2/44
- https://www.mdpi.com/1420-3049/26/6/1649
- https://onlinelibrary.wiley.com/doi/10.1111/exd.14331
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11450438/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9321855/
- https://www.ocl-journal.org/articles/ocl/pdf/2004/06/ocl2004116p401.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6139190/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10841493/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8155912/
- http://www.jlr.org/content/48/12/2531.full.pdf
- http://www.clausiuspress.com/conferences/AEASR/FBB 2020/FBB2020029.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8000920/
- https://www.hindawi.com/journals/jl/2018/5954034/
- https://pubmed.ncbi.nlm.nih.gov/26844894/
- https://www.nature.com/articles/s41598-023-47051-6
- https://learning-center.homesciencetools.com/article/skin-touch/
- https://pubmed.ncbi.nlm.nih.gov/24252189/
- https://onlinelibrary.wiley.com/doi/10.1111/jdv.18123
- https://en.wikipedia.org/wiki/Mechanoreceptor
- https://onlinelibrary.wiley.com/doi/10.1111/bjd.20955
- https://www.oncobeta.com/your-health/nmsc-info/the-skin
- https://courses.lumenlearning.com/wm-biology2/chapter/somatosensory-receptors/
- https://academic.oup.com/bjd/advance-article/doi/10.1093/bjd/ljaf200/8142502?searchresult=1
- https://www.kenhub.com/en/library/physiology/peripheral-mechanosensory-receptors
- https://www.mollenol.com/q-a/understanding-pimples-and-the-role-of-mollenol/
- https://www.mollenol.com/forum/about-mollenol/
- https://www.mdpi.com/1420-3049/29/5/999
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7227856/
- https://www.clinikally.com/blogs/news/lauric-acid-the-unsung-hero-of-healthy-radiant-skin
- https://elchemy.com/blogs/personal-care/lauric-acid-and-coconut-oil-the-science-behind-their-powerful-combination
- https://pubmed.ncbi.nlm.nih.gov/7576514/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10295805/
- https://www.tandfonline.com/doi/full/10.1080/13880209.2017.1312464
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7011944/
- https://www.mdpi.com/1420-3049/28/6/2872
- https://www.mdpi.com/1999-4923/17/6/793
- https://www.healthline.com/nutrition/top-10-evidence-based-health-benefits-of-coconut-oil
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8036490/
- https://www.tandfonline.com/doi/full/10.1080/17568919.2024.2419376
- https://www.mdpi.com/2218-0532/90/1/14
- https://www.dermatoljournal.com/articles/essential-oils-as-skin-permeation-boosters-and-their-predicted-effect-mechanisms.html
- https://www.mollenol.com/how-to-use/
- >
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11663679/
- https://iaesprime.com/index.php/csit/article/view/194
- https://www.ewadirect.com/proceedings/tns/article/view/17176
- https://www.mdpi.com/2079-9284/8/3/66
- https://ijarsct.co.in/Paper24848.pdf
- https://ijcap.in/article-details/20604
- https://journals.sagepub.com/doi/10.1177/1934578X251353560
- https://www.mdpi.com/1660-3397/17/12/688
- https://www.mdpi.com/1422-0067/18/1/175/pdf
- https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/jocd.15976
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11942248/
- https://www.mdpi.com/1420-3049/25/11/2536/pdf
- https://www.mdpi.com/2079-9284/8/3/89/pdf
- https://www.mdpi.com/2079-9284/9/1/3/pdf?version=1640605926
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11990743/
- https://www.mdpi.com/1420-3049/28/2/534/pdf?version=1672916408
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7321322/
- https://timesofindia.indiatimes.com/life-style/food-news/heres-how-clove-oil-is-beneficial-for-your-skin/articleshow/68181978.cms
- https://www.mollenol.com/common-skin-problems/
- https://www.mdpi.com/2310-2861/10/4/227
- https://linkinghub.elsevier.com/retrieve/pii/S2949824425000370
- https://www.pubhort.org/fruits/75/5/5/index.htm
- https://jurnal.ugm.ac.id/v3/JFPS/article/view/15875
- https://dx.plos.org/10.1371/journal.pone.0313517
- https://www.preprints.org/manuscript/202010.0189/v1
- http://link.springer.com/10.1007/978-981-15-1664-1_16
- https://www.mdpi.com/1999-4923/17/7/852
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10974782/
- https://microbiologyjournal.org/download/90092/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6274078/
- https://eurekabiomedical.com/index.php/EHI/article/download/18/28
- https://www.mdpi.com/1420-3049/29/6/1225/pdf?version=1709913973
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5880794/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8267472/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11761885/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9171427/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11698606/
- https://journals.cambridgemedia.com.au/wpr/volume-27-number-4/antimicrobial-and-healing-promoting-properties-animal-and-plant-oils-treatment-infected-wounds
- https://www.sciencedirect.com/science/article/abs/pii/B9780323851770000197
- https://allmedic.net.au/blogs/news/the-truth-about-tea-tree-oil-for-acne
- http://www.tandfonline.com/doi/full/10.1080/10717540500395064
- https://link.springer.com/10.1007/978-3-662-47039-8_11
- https://journals.lww.com/10.4103/2311-8571.351508
- https://linkinghub.elsevier.com/retrieve/pii/0378517389903104
- https://link.springer.com/10.1007/s13346-025-01809-9
- https://linkinghub.elsevier.com/retrieve/pii/S0378517322000941
- https://www.tandfonline.com/doi/pdf/10.1080/13880209.2017.1312464?needAccess=true
- https://www.mdpi.com/2218-0532/90/1/14/pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12044306/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11859311/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4228507/
- https://www.mdpi.com/2079-9284/8/2/36/pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9223005/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9331963/
- https://www.letsmakebeauty.com/blog/post/why-your-skincare-needs-penetration-enhancers-maximizing-active-performance
- https://www.webmd.com/skin-problems-and-treatments/acne/what-are-hydrocolloid-patches-for-pimples
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1276383/full
- https://www.sciencedirect.com/science/article/pii/S1319562X19302414
- https://consensus.app/search/what-are-the-most-effective-skin-penetration-enhan/solNHfEiRE-vMGIS3bJqQg/
