How to Strengthen Skin Barrier: Ingredients, Routine, Diet
5th Oct 2025
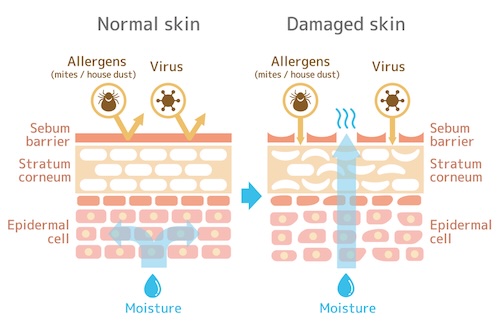 If your face feels tight after cleansing, stings when you apply products, or looks dull no matter how much moisturizer you use, your skin barrier may need help. Your “skin barrier” is the outermost layer of skin (the stratum corneum) plus its slightly acidic film (the acid mantle). Think of it as a brick‑and‑mortar wall: flat skin cells are the bricks, and lipids like ceramides, cholesterol, and fatty acids are the mortar. When this wall is intact, it keeps moisture in and irritants, allergens, and microbes out. When it’s weakened, water escapes, irritants sneak in, and sensitivity flares.
If your face feels tight after cleansing, stings when you apply products, or looks dull no matter how much moisturizer you use, your skin barrier may need help. Your “skin barrier” is the outermost layer of skin (the stratum corneum) plus its slightly acidic film (the acid mantle). Think of it as a brick‑and‑mortar wall: flat skin cells are the bricks, and lipids like ceramides, cholesterol, and fatty acids are the mortar. When this wall is intact, it keeps moisture in and irritants, allergens, and microbes out. When it’s weakened, water escapes, irritants sneak in, and sensitivity flares.
This guide shows you exactly how to strengthen your skin barrier with ingredients, routines, and diet that are backed by dermatology basics. You’ll learn the signs of a compromised barrier, what commonly damages it, why pH matters, and which ingredients rebuild it fastest. We’ll cover humectants vs. occlusives, soothing actives to use, what to scale back, step‑by‑step routines by skin type, patch testing, sun protection, shopping tips, nutrition and supplements, daily habits, and realistic repair timelines. You’ll also find barrier‑safe tips if you’re managing skin infections like molluscum, folliculitis, or acne, plus when to see a dermatologist. Let’s start with how to spot the problem.
Signs your skin barrier is compromised
Your barrier’s job is to keep water in and irritants and microbes out. When that “brick-and-mortar” wall thins or gaps, water loss rises and the stratum corneum dehydrates. Clinically, this shows up as higher transepidermal water loss (TEWL) and lower surface hydration; day to day, you’ll notice comfort and appearance changes that don’t resolve with your usual moisturizer.
- Dry, scaly, or flaky skin: Feels rough and looks dull despite moisturizing.
- Tightness, stinging, or burning after mild products: A hallmark of heightened sensitivity.
- Redness and inflammation: Easily irritated patches that feel warm or tender.
- Itchiness: Often worse in dry rooms or after hot showers.
- Rough or discolored patches: Uneven tone or texture, especially around the nose, cheeks, and chin.
- Acne or more frequent breakouts: A disrupted barrier can aggravate blemishes.
- More skin infections: Bacterial, viral, or fungal rashes occur or linger more than usual.
- Oily but dehydrated feel: Skin looks shiny yet feels parched and tight underneath.
- Makeup pilling or patchiness: Products won’t sit smoothly or soak in evenly.
If you’re nodding to several of these, it’s time to focus your routine on how to strengthen the skin barrier. Next, here’s what commonly chips away at it in the first place.
What damages the skin barrier
Before you can fix a fragile barrier, it helps to name the culprits. The outer “brick-and-mortar” layer is constantly defending you from the environment and your own habits. Repeated hits—think harsh cleansers, too much sun, or scrubbing—create tiny gaps that raise transepidermal water loss (TEWL) and leave skin touchy and dehydrated. Knowing what to limit is the first step in how to strengthen your skin barrier.
- Climate extremes: Very dry or very humid air, wind, and indoor heating/AC dehydrate or swell the stratum corneum, weakening cohesion.
- UV exposure: Too much sun disrupts lipids and proteins, fueling inflammation and pigment changes.
- Alkaline soaps and detergents: High‑pH cleansers strip essential lipids and disturb the acid mantle.
- Overwashing and overexfoliating: Frequent cleansing, strong acids, scrubs, or brushes raise TEWL and sensitivity.
- Harsh chemicals and irritants: Solvents, household cleaners, allergens, and pollutants provoke irritation and barrier disruption.
- Prolonged hot water: Long, hot showers and soaking impair barrier lipids and hydration.
- Steroids (misused or long‑term): Topical or systemic steroids can thin skin and compromise barrier function.
- Psychological stress: Stress can worsen inflammation and impair repair processes.
- Genetics and skin conditions: Atopic dermatitis and psoriasis predispose to barrier defects.
Next, a key piece many routines miss: why pH and your acid mantle matter so much to barrier strength.
Why pH and the acid mantle matter
Your skin’s acid mantle is a thin, slightly acidic film that sits on top of the “brick-and-mortar” barrier. In healthy skin it hovers around pH 4.0–5.8, which keeps key enzymes humming, lipids organized, and friendly microbes in charge. When pH drifts upward (think alkaline soaps or harsh detergents), enzymes misfire, inflammatory proteases switch on, and less-helpful bacteria gain ground. The result: higher transepidermal water loss (TEWL), more sting and redness, and slower recovery—especially around wounds, where acidity supports healing.
To use pH to your advantage while you work on how to strengthen the skin barrier, make these simple, pH-smart moves part of your routine:
- Choose a low‑pH cleanser (about 4–5): “pH-balanced” can be vague; look for gentle, non-alkaline formulas and skip traditional alkaline bar soaps.
- Wash with lukewarm water and pat dry: Overwashing or hot water can disrupt the mantle and raise TEWL.
- Go easy on exfoliation: Introduce mild chemical exfoliants slowly; harsh scrubs can spike irritation and pH.
- Prefer leave‑ons near skin pH: Moisturizers and serums formulated close to skin’s acidity help maintain the mantle while ceramides and humectants rebuild lipids and hydration.
- Consider health factors: Conditions like diabetes or incontinence can shift skin pH—slightly more acidic products may help; ask your clinician.
Next up: the core ingredients that actively rebuild the barrier’s “mortar.”
Core ingredients that rebuild the skin barrier
When you’re serious about how to strengthen skin barrier function, think like a mason: refill the “mortar” (lipids), draw in water, then seal it. Choose formulas that mimic what naturally lives in the stratum corneum and respect your acid mantle so repair can keep pace with daily wear and tear.
-
Ceramides: These waxy lipids are foundational to barrier integrity. Products featuring ceramides (and even pseudo‑ceramides) have been shown to ease dryness, itch, and scaling, especially in sensitive, eczema‑prone skin.
-
Cholesterol + fatty acids: Alongside ceramides, these lipids help rebuild the lamellar layers that lock moisture in. Look for moisturizers that combine all three—ceramides, cholesterol, and fatty acids—to mirror skin’s natural composition.
-
Petrolatum (occlusive): A powerhouse sealer that can block up to 99% of water loss when used as the final step. Target very dry, chapped, or post‑procedure areas to quickly reduce transepidermal water loss (TEWL).
-
Humectants (water magnets): Hyaluronic acid, glycerin, honey, and urea pull water into the stratum corneum and support enzyme activity that keeps the barrier flexible. Pair humectants with an occlusive or rich cream to prevent evaporation.
-
Barrier‑friendly plant oils: Research suggests oils like jojoba, sunflower, argan, borage, coconut, almond, and soybean can help repair the barrier, limit moisture loss, and provide antibacterial, anti‑inflammatory, and antioxidant benefits. Apply alone or within a cream—and patch test first if you’re sensitive.
-
pH‑smart bases: Formulas near skin’s natural acidity (about pH 4–5) help maintain the acid mantle so lipids organize and microbes stay in balance while you rebuild.
Stacking these categories—lipids + humectants + a smart seal—is the fastest, most reliable path for how to strengthen the skin barrier. Up next, we’ll help you choose the right moisturizer by decoding humectants versus occlusives and when to use each.
Humectants vs occlusives: choosing the right moisturizer
The fastest way to strengthen the skin barrier is to both add water and stop it from escaping. Humectants pull water into the stratum corneum; occlusives slow transepidermal water loss (TEWL) by sealing it in. Pair them wisely and you’ll notice less tightness, less sting, and a healthier, springier feel.
| What it is | How it works | Examples | Best for | Watch-outs |
|---|---|---|---|---|
| Humectant | Draws water from air or deeper layers into the outer skin | Hyaluronic acid, glycerin, honey, urea | Dehydrated, tight skin; under a cream | In very dry air, always top with a cream/occlusive to prevent evaporation |
| Occlusive | Forms a thin film to reduce water loss | Petrolatum, mineral oil, plant waxes | Very dry, chapped, post-procedure areas | Can feel greasy; use thinly, especially on acne-prone zones |
How to choose and use for barrier repair:
- Very dry or compromised barrier: Apply a humectant serum, then a ceramide-rich cream, then spot‑seal with a thin layer of petrolatum at night. Petrolatum can block up to 99% of water loss when used as the final step.
- Oily or acne‑prone but dehydrated: Use a light humectant (hyaluronic acid or glycerin) and a non‑comedogenic gel‑cream; reserve occlusives for corners of the nose or lips only.
- Cold or very dry climate/indoors with heating: Favor creams/ointments with fatty acids, cholesterol, and ceramides over gels; always “top” humectants.
- Humid climate: A humectant plus a lightweight emulsion may suffice; add an occlusive only on hot spots (cheeks, around the mouth).
- After cleansing: Pat skin damp, apply humectant within 60 seconds, then your cream; finish with a targeted occlusive where needed.
This simple stack—humectant to hydrate, emollient/ceramides to rebuild, occlusive to seal—is your day‑one plan for how to strengthen skin barrier without overcomplicating your routine.
Supportive actives that calm and repair
While you rebuild the “mortar,” add soothing, low‑irritation actives that dial down inflammation and nudge skin to make more of its own lipids and barrier proteins. Keep formulas fragrance‑free and pH‑smart so you’re not undoing your progress as you work on how to strengthen the skin barrier.
-
Niacinamide (vitamin B3): Supports key barrier lipids like ceramides and fatty acids, helping reduce redness and improve resilience over time.
-
Probiotic/postbiotic lysates: Early studies in skin models show certain Lactobacillus lysates can reduce pro‑inflammatory signals and boost barrier proteins (like filaggrin, loricrin, and aquaporin‑3), suggesting a calming, strengthening effect.
-
Prebiotic/synbiotic support (emerging): In small human trials, a prebiotic (GOS) paired with probiotic milk improved skin hydration; we expand on diet‑based options later.
-
Barrier‑friendly plant oils: Jojoba, sunflower, argan, borage, coconut, almond, and soybean oils can help repair the barrier, curb moisture loss, and offer antibacterial, anti‑inflammatory, and antioxidant benefits. Patch test first.
-
Humectants that soothe: Hyaluronic acid, glycerin, honey, and urea draw water into the stratum corneum and support flexibility. Always follow with a cream to keep that water in.
-
Pseudo‑ceramides: Shown to ease dryness, itch, and scaling in sensitive, eczema‑prone skin by mimicking natural ceramides.
-
Targeted occlusion: A thin layer of petrolatum over irritated spots at night can sharply reduce transepidermal water loss and calm sting while you sleep.
Use one or two of these at a time alongside your core ceramide‑rich moisturizer; simplicity speeds recovery. Next, here’s what to scale back while your barrier heals.
Ingredients and treatments to scale back while repairing
When your barrier is leaky, the fastest way to feel better is to remove what keeps poking holes in it. For a few weeks, think “gentle, low‑pH, minimal.” This reduces transepidermal water loss (TEWL), lets lipids reorganize, and speeds the outcome you want: calm, comfortable skin that holds water again.
- Alkaline soaps/detergents: High‑pH cleansers disrupt the acid mantle. Swap to low‑pH (about 4–5) gentle cleansers.
- Overwashing and hot water: Limit cleansing to 1–2×/day, keep showers short, and use lukewarm water.
- Overexfoliation: Pause scrubs, spinning brushes, and strong acids. The AAD notes scrubs/brushes can damage the barrier; sensitive types should use a soft cloth and, if needed, a mild chemical exfoliant later.
- Harsh chemicals/irritants: Minimize contact with solvents, household cleaners, and known allergens/pollutants that provoke irritation.
- UV overexposure: Don’t skip sunscreen while healing—excess sun disrupts barrier lipids and proteins.
- Prolonged or unsupervised steroid use: Extended topical/systemic steroid use can thin skin and impair the barrier; use only as directed by your clinician.
- Anything that stings or burns: Persistent sting is your cue to stop and reintroduce later after recovery.
- Frequent product turnover: Avoid adding multiple new products during repair; keep the routine simple and stable.
Scale back to a core: gentle cleanse, humectant, ceramide‑rich moisturizer, and strategic occlusion. This “subtraction first” approach is foundational to how to strengthen the skin barrier—then add back actives slowly once comfort and hydration are steady.
Step-by-step routine to repair your skin barrier (by skin type)
Keep it minimal, pH‑smart, and consistent. Across all skin types, the fastest path for how to strengthen skin barrier function is the same stack: gentle low‑pH cleanse, humectant to hydrate, ceramide‑rich moisturizer to rebuild, and targeted occlusion to seal. Use lukewarm water, fragrance‑free formulas, and pause strong exfoliants while you heal.
Dry or dehydrated
Focus on drawing in water and preventing escape to lower TEWL and tightness.
- AM
- Gentle cleanse (low pH ~4–5) or rinse.
- Humectant (hyaluronic acid, glycerin, urea) on damp skin.
- Ceramide + cholesterol + fatty acid cream.
- Sunscreen (details in section below).
- PM
- Gentle cleanse.
- Humectant, then a richer ceramide cream.
- Spot occlude with petrolatum on cracks/chapped areas to reduce up to 99% water loss.
Oily or acne‑prone (but dehydrated)
Hydrate lightly, rebuild lipids, and seal only where needed to avoid heaviness.
- AM
- Low‑pH gel cleanser.
- Light humectant layer.
- Non‑comedogenic gel‑cream with ceramides.
- Sunscreen.
- PM
- Low‑pH cleanse.
- Humectant, then light ceramide moisturizer.
- Micro‑occlude only dry corners (nostrils/lips); avoid thick occlusives on the T‑zone.
Combination
Treat zones differently: cushion dry areas and keep oily areas light.
- AM
- Gentle cleanse.
- Humectant all over.
- Cream on cheeks/jaw; gel‑cream on T‑zone.
- Sunscreen.
- PM
- Gentle cleanse.
- Humectant, then ceramide cream on dry patches and lighter lotion on oily zones.
- Petrolatum spot seal only where flaky.
Sensitive or eczema‑prone
Minimize steps, respect the acid mantle, and lean on barrier lipids and soothing oils.
- AM
- Creamy, low‑pH cleanser or rinse.
- Ceramide‑rich moisturizer (fragrance‑free).
- Optional: few drops of barrier‑friendly oil (sunflower, jojoba) mixed into cream.
- Sunscreen.
- PM
- Gentle cleanse.
- Ceramide moisturizer, then petrolatum over hot spots to curb sting and water loss.
- Keep formulas fragrance‑free and avoid scrubs/brushes until calm.
Stick with this simplified plan daily for several weeks before slowly reintroducing actives (next section shows how to patch test and pace it).
How to patch test and introduce products safely
When your barrier is fragile, the goal is zero surprises. Patch testing lets you screen for irritation before you put a new product all over your face. Go slow, add one thing at a time, and favor low‑pH, fragrance‑free formulas while you work on how to strengthen the skin barrier.
- Choose a test spot: inner forearm or behind the ear on clean, dry skin.
- Apply a pea‑size amount (or 1–2 drops). Leave on; don’t cover or wash off for 24 hours. For cleansers, use as directed, then monitor.
- Watch for signs of trouble: persistent stinging, itching, redness, swelling, or new bumps during the next 24–48 hours. If present, stop.
- If clear, do a “use test”: apply to a small facial area once daily for 3 days. If still calm, expand to the whole face.
- Introduce only one new product every 3–7 days so you can pinpoint reactions and avoid overloading the barrier.
- Start low and slow with actives: acids or retinoids 1–2×/week at night; buffer by applying moisturizer first; increase frequency only if comfortable.
- Sensitive or eczema‑prone? Extend patch testing to 48 hours, avoid scrubs/brushes, and prioritize ceramides, humectants, and gentle plant oils (patch test oils first).
- Any reaction that lasts beyond 24 hours, or any blistering, requires a pause; return to your core routine (cleanser, ceramide moisturizer, targeted occlusion) until calm.
This deliberate pace prevents setbacks and keeps your progress steady.
Sun protection basics for a stronger barrier
UV exposure is a top barrier saboteur. It disrupts lipids and proteins in the “mortar,” fuels inflammation, and can raise transepidermal water loss, leaving skin stingy and dehydrated. While you work on how to strengthen skin barrier function with gentle cleansers, humectants, and ceramides, daily sun protection helps preserve repairs and prevents new damage.
- Limit direct sun when you can: Favor shade and shorter exposures while your skin is sensitized.
- Pick gentle, fragrance‑free formulas: If sunscreen stings, switch textures (cream for dry, gel for oily) and patch test first.
- Apply as the last AM step: Layer over your moisturizer to form an even, comfortable film on all exposed skin.
- Use enough and be consistent: Cover face, neck, and ears; reapply as directed on the label during prolonged time outside.
- Buffer if you’re reactive: Apply moisturizer first, then sunscreen; this often reduces sting without undermining protection.
- After sun, replenish: Cleanse gently, then rebuild with humectants and ceramide‑rich creams; spot‑seal dry patches with a thin layer of petrolatum.
Sunscreen is one pillar; pairing it with smart behavior (timing, shade) keeps your progress steady and speeds comfortable, resilient skin.
How to shop for barrier-friendly skin care
Faced with a wall of bottles, shop like a “barrier builder.” Prioritize formulas that respect your acid mantle (pH ~4–5), refill skin lipids (ceramides, fatty acids, cholesterol), add water (humectants), and seal it in (occlusives). This simple filter prevents products that spike irritation or raise transepidermal water loss.
- Start with a low‑pH cleanser (about 4–5): Skip alkaline bar soaps and harsh detergents that disturb the acid mantle; look for gentle, non‑alkaline wording and pH info when brands provide it.
- Pick a ceramide‑rich moisturizer: Best if it also lists cholesterol and fatty acids to mirror skin’s natural “mortar.” Pseudo‑ceramides are helpful too for dryness, itch, and scaling.
- Ensure humectants are inside: Hyaluronic acid, glycerin, honey, or urea draw water into the stratum corneum; pair them with a cream so moisture doesn’t evaporate.
- Add an occlusive for nights or hot spots: A thin layer of petrolatum over dry, chapped areas can block up to 99% of water loss and quickly reduce sting.
- Consider barrier‑friendly plant oils: Jojoba, sunflower, argan, borage, coconut, almond, soybean may aid repair and calm inflammation. Patch test first if you’re reactive.
- Favor simple, gentle formulas: Fragrance‑free options and minimal actives reduce the risk of flare while you rebuild.
- Shop by climate/skin feel: Drier air calls for creams/ointments; humid weather may do better with gel‑creams plus targeted occlusion.
A practical starter kit: low‑pH cleanser + ceramide moisturizer (with humectants) + petrolatum for spot‑sealing; optionally layer a patch‑tested plant oil. Keep receipts, patch test new items, and introduce only one product at a time to protect your progress while you work on how to strengthen the skin barrier.
Diet and supplements for barrier health
Your skin builds its “mortar” from what you eat, and your gut microbiome talks to your skin’s immune and chemical layers. Small human trials suggest diet can raise stratum corneum hydration and reduce transepidermal water loss (TEWL), but effects are modest and take consistency. Treat nutrition as a steady assist—not a quick fix—while you work on how to strengthen skin barrier with smart topical care.
What to eat more often
- Omega‑3 sources: Fatty fish, flaxseed, chia, walnuts. A higher omega‑3 to omega‑6 balance is associated with better barrier function. In trials, flaxseed oil rich in ALA improved TEWL, hydration, scaling, and roughness over 12 weeks.
- Fermented and fiber‑rich foods: Plain yogurt/kefir with live cultures and prebiotic fibers (such as galacto‑oligosaccharides in foods/supplements) support gut microbes that produce short‑chain fatty acids tied to stronger epithelial barriers. A synbiotic drink (probiotic milk + GOS) improved skin hydration in a small study.
- Healthy oils and antioxidants: Use a variety of unsaturated plant oils in cooking and pile on colorful produce to help counter inflammation that chips at the barrier.
- Hydration: Staying well hydrated supports stratum corneum flexibility and comfort.
Supplements with the most evidence (small trials)
- Omega‑3s: Plant (flaxseed oil/ALA) and marine omega‑3s (EPA/DHA) have shown improvements in hydration, TEWL, and clinical dryness in some studies. Hempseed oil (omega‑6:omega‑3 ~2:1) improved dryness in atopic skin, though TEWL changes were inconsistent.
- Probiotics/prebiotics/synbiotics: Oral Lactobacillus strains have reduced TEWL and increased hydration in RCTs; GOS prebiotic plus probiotic milk improved hydration.
- GLA oils (evening primrose, borage): Mixed results; some studies report TEWL benefits, others show no difference. May help select people (baseline fatty‑acid status matters).
- L‑histidine: In a small RCT of adults with eczema, daily l‑histidine increased filaggrin formation and improved barrier function.
How to use them wisely
- Think timelines: Trials commonly ran 4–12 weeks; reassess after one bottle/one bag of capsules, not one week.
- Go one at a time: Add a single supplement so you can gauge benefit and tolerance.
- Check with your clinician: Especially if pregnant, nursing, on medications, or managing medical conditions.
Used alongside low‑pH cleansing, ceramides, humectants, and smart occlusion, nutrition can gently tilt the odds toward a calmer, better‑sealed barrier.
Daily habits that protect your barrier
Strong skin starts with small, repeatable choices. Gentle daily habits lower transepidermal water loss (TEWL), keep your acid mantle in its sweet spot, and give the “brick‑and‑mortar” lipids time to rebuild. You don’t need a 10‑step routine—just consistent, low‑irritation moves that stack up.
- Keep showers short and lukewarm: Long, hot water strips lipids. Pat dry and moisturize within 60 seconds to trap water.
- Cleanse smart, not more: Once nightly (AM rinse if needed) with a low‑pH (~4–5) gentle cleanser; skip alkaline bar soaps and harsh detergents.
- Moisturize twice daily: Layer humectants (hyaluronic acid, glycerin, urea) under a ceramide + fatty acid + cholesterol cream. Spot‑seal with petrolatum at night—studies show it can block up to 99% of water loss.
- Be sun‑savvy every day: Limit direct midday sun and apply sunscreen as your last AM step to protect newly rebuilt lipids.
- Go easy on exfoliation: Pause scrubs/brushes. If you reintroduce later, use a soft cloth and a mild chemical exfoliant sparingly.
- Limit irritants: Wear gloves for cleaning, avoid known allergens/solvents, and choose fragrance‑free laundry and skin care.
- Tune your environment: Dry or overly humid air stresses skin; use a humidifier in dry seasons and avoid steamy, prolonged baths.
- Mind stress, move, hydrate, and eat well: Psychological stress impairs repair. Daily movement supports circulation; drink water; prioritize omega‑3s and fermented/prebiotic foods to support barrier function.
- Reapply where it counts: Hands and lips take a beating—moisturize after washing and occlude lips as needed.
- Listen to your skin: If a product stings or burns, stop and return to your core routine while you heal.
How long skin barrier repair takes
Most barriers don’t break in a day, and they don’t heal overnight—but with a gentle, pH‑smart routine, comfort usually improves fast. Expect symptom relief (less sting and tightness) within days, with meaningful repair over weeks. Small clinical trials and expert guidance suggest early improvement in a few days and typical recovery in about 2–4 weeks when triggers are removed and lipids/hydration are restored. Diet and supplement changes generally need longer, often 4–12 weeks, to show skin effects.
- 24–72 hours: Sting and redness ease as you switch to low‑pH cleansing, add humectants, and seal with a ceramide cream; targeted petrolatum can cut water loss overnight.
- 7 days: Tightness decreases; flakes soften; makeup sits better. Sensitivity after cleansing should drop.
- 2–4 weeks: Barrier feels “quiet” and holds water again; fewer flare‑ups; less need to reapply moisturizer.
- 8–12 weeks: Nutrition shifts (omega‑3s, synbiotics) begin to reflect in hydration/TEWL changes seen in small trials.
What speeds repair: consistent routine, low‑pH cleanser, ceramides + fatty acids + cholesterol, humectants topped with a cream, sun protection, and avoiding over‑exfoliation. What slows it: harsh/alcohol‑heavy or alkaline products, hot water, climate extremes, stress, and conditions like eczema or diabetes. If irritation persists or worsens despite a simplified routine, pause new actives and consider professional guidance.
Barrier care when you have skin infections such as molluscum, folliculitis, or acne
Infections and a fragile barrier often fuel each other. Over‑cleansing, scrubbing, and harsh spot treatments raise transepidermal water loss (TEWL), sting, and slow healing. Your strategy: treat the bumps while protecting the acid mantle (pH ~4–5), replenishing lipids, and minimizing friction so skin can re‑seal.
Molluscum contagiosum
Molluscum is viral and common in kids; the priority is comfort, coverage, and preventing spread from scratching. Keep routines gentle and consistent around lesions.
- Cleanse low‑pH and lukewarm: Skip alkaline soaps and hot water to preserve the mantle.
- Moisturize the surrounding skin: Use a fragrance‑free ceramide + fatty acid + cholesterol cream to reduce itch and protect nearby skin.
- Cover to protect: Hydrocolloid patches cushion bumps, reduce picking and friction, and create a clean micro‑environment—change as directed.
- Spot‑soothe smartly: A thin layer of petrolatum on adjacent chapped areas can block up to 99% of water loss overnight without adding sting.
Folliculitis
When follicles are inflamed, friction and occlusion make it worse. Keep the barrier calm and the texture breathable.
- Gentle, low‑pH cleansing: Once daily (AM rinse if needed); avoid brushes and scrubs.
- Light, non‑occlusive hydration: Layer a humectant (hyaluronic acid or glycerin) under a non‑comedogenic ceramide gel‑cream.
- Target the bumps, not the whole area: Use hydrocolloid patches on pus‑filled bumps; avoid heavy oils and thick ointments over clusters.
Acne
Acne‑prone skin is often dehydrated from over‑treatment. Rebuild first; then reintroduce actives slowly.
- Simplify: Low‑pH gel cleanser, humectant on damp skin, then a lightweight ceramide moisturizer; daily sunscreen that feels comfortable.
- Spot care with less trauma: Hydrocolloid patches over whiteheads help protect from picking while maintaining a cleaner surface.
- Seal selectively: If needed, micro‑occlude only non‑acne dry corners (nostrils, lips); keep thick occlusives off congested zones.
- Plant oils with care: Some barrier‑friendly oils (like jojoba or sunflower) can be helpful—always patch test first and use sparingly.
This balanced approach—pH‑smart cleansing, ceramide‑rich moisture, strategic patching, and minimal friction—lets you address bumps while steadily strengthening the skin barrier.
When to see a dermatologist
Most weakened barriers start to feel better within days and stabilize over 2–4 weeks when you switch to a gentle, low‑pH routine with humectants and ceramides. If that’s not happening—or if you’re dealing with infections or chronic conditions—professional care can prevent setbacks and scarring.
- No improvement or worsening in 2–4 weeks: Persistent sting, redness, flaking, or new breakouts despite a simplified routine.
- Severe or acute symptoms: Diffuse swelling, oozing/crusting, intense burning, or pain.
- Frequent infections: Recurrent bacterial, viral, or fungal rashes; molluscum spreading or lesions near the eyes/genitals; folliculitis with fever or painful nodules; acne with cysts or scarring risk.
- Underlying conditions: Atopic dermatitis, psoriasis, diabetes, or immunocompromised states that can alter pH and slow healing.
- Steroid questions: Need guidance on starting, tapering, or avoiding long‑term topical steroid use.
- Suspected contact allergy: You may need formal patch testing to identify triggers (fragrance, preservatives, detergents).
- Children and infants: Rapidly spreading rashes, sleep‑disturbing itch, or lesions in sensitive areas warrant prompt evaluation.
- Non‑healing wounds or post‑procedure care: Areas that won’t close or stay irritated.
A dermatologist can tailor pH‑appropriate care, select barrier‑repair topicals (including ceramides/pseudo‑ceramides), treat infections, and create a plan that rebuilds your “brick‑and‑mortar” without unnecessary irritation.
Quick answers to common questions
You don’t need a 10-step routine to get results. These fast, evidence‑based answers focus on what reliably works when you’re figuring out how to strengthen skin barrier function without setbacks.
-
How do I know my barrier is damaged? Dryness, tightness/sting after mild products, redness, itch, flaking, more breakouts, and more frequent skin infections are common signs.
-
What’s the fastest way to feel better? Switch to a low‑pH (≈4–5) gentle cleanser, apply humectants, a ceramide‑rich cream, then spot‑seal with petrolatum at night.
-
Which ingredients help most? Ceramides + cholesterol + fatty acids, humectants (hyaluronic acid, glycerin, urea, honey), petrolatum, and patch‑tested plant oils (jojoba, sunflower, argan, borage, coconut, almond, soybean).
-
Is petrolatum (Vaseline) okay? Yes—used thinly, it can block up to 99% of water loss; avoid heavy layers on acne‑prone zones.
-
What cleanser pH should I use? Aim for low pH (~4–5) to support the acid mantle (normal skin pH ~4.0–5.8).
-
Should I exfoliate while repairing? Pause scrubs/brushes; if needed later, reintroduce a mild chemical exfoliant slowly and infrequently.
-
Can oily/acne‑prone skin moisturize? Yes; use a non‑comedogenic gel‑cream with ceramides and seal only dry corners.
-
Do diet and supplements help? Small trials suggest omega‑3s (e.g., flaxseed oil), probiotics/prebiotics/synbiotics, and in some cases GLA oils can improve hydration/TEWL; think 4–12 weeks.
-
How long does repair take? Comfort often improves in days; typical recovery is ~2–4 weeks with a gentle, consistent routine.
-
Does sunscreen matter during repair? Absolutely—UV disrupts barrier lipids; apply a comfortable, fragrance‑free sunscreen daily as your last AM step.
Key takeaways
Stronger skin isn’t about more products—it’s about the right ones used consistently. Keep your acid mantle happy, refill the “mortar,” add water, and stop it from escaping. With a low‑pH cleanse, smart moisturizing stack, and sun sense, most people feel better fast and see steady repair in weeks.
- Start simple: Low‑pH (≈4–5) gentle cleanser, lukewarm water, short showers.
- Rebuild the “mortar”: Use ceramides + cholesterol + fatty acids daily.
- Hydrate, then seal: Layer humectants, a cream, then thin petrolatum at night.
- Protect every morning: Comfortable sunscreen plus smart shade habits.
- Pause irritants: Hot water, scrubs/brushes, strong acids, alkaline soaps.
- Go slow with actives: Patch test and add one product every 3–7 days.
- Support with diet: Prioritize omega‑3s and fermented/prebiotic foods; think 4–12 weeks.
- Timeline: Comfort in days; typical recovery in 2–4 weeks—see a derm if not improving.
Managing bumps like molluscum, folliculitis, or acne? Pair this barrier routine with gentle coverage and targeted spot care. For home options—including hydrocolloid patches and sensitive‑area treatments—visit Mollenol.
